Nursing diagnosis for hiatal hernia plays a crucial role in guiding patient care and management. This comprehensive guide delves into the intricacies of hiatal hernia, encompassing its definition, assessment techniques, nursing interventions, and patient education strategies.
Understanding the pathophysiology and clinical presentation of hiatal hernia is essential for accurate nursing diagnosis. This guide provides a detailed overview of the condition, enabling nurses to make informed decisions and develop effective care plans.
Overview of Hiatal Hernia
A hiatal hernia occurs when part of the stomach protrudes through an opening in the diaphragm, the muscle that separates the chest cavity from the abdominal cavity. This opening, called the hiatus, normally allows the esophagus to pass through. Hiatal hernias are common, affecting up to 60% of people over the age of 50.
There are two main types of hiatal hernias: sliding hernias and paraesophageal hernias. Sliding hernias occur when the stomach slides up into the chest cavity through the hiatus. Paraesophageal hernias occur when the stomach protrudes through the hiatus alongside the esophagus.
Nursing Assessment
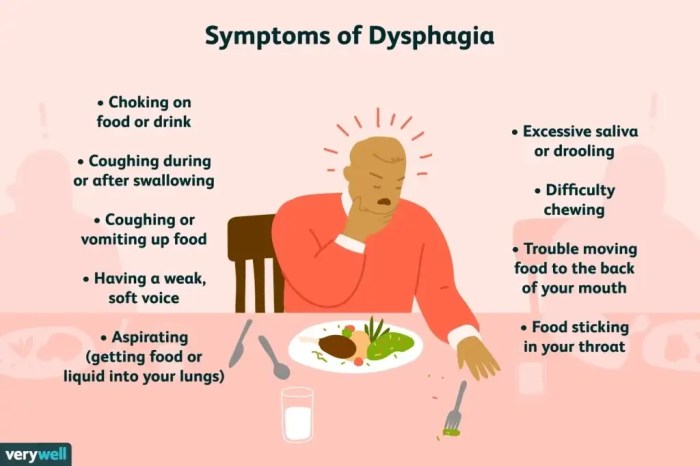
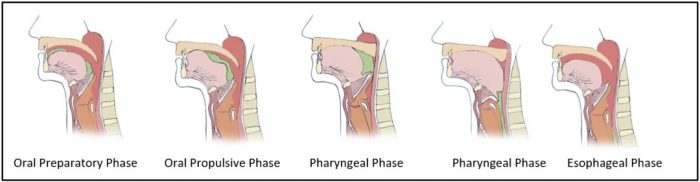
A thorough nursing assessment is essential for diagnosing a hiatal hernia. Subjective assessment findings may include heartburn, regurgitation, difficulty swallowing, and chest pain. Objective assessment findings may include a visible bulge in the upper abdomen, tenderness on palpation, and a positive cough impulse.
A physical examination can be performed to assess for a hiatal hernia. The nurse should auscultate for bowel sounds in the chest cavity, percuss for tympany, and palpate for a mass in the upper abdomen.
A thorough nursing history is also important in diagnosing a hiatal hernia. The nurse should ask about the patient’s symptoms, as well as any risk factors for developing a hiatal hernia, such as obesity, smoking, and pregnancy.
Nursing Diagnosis
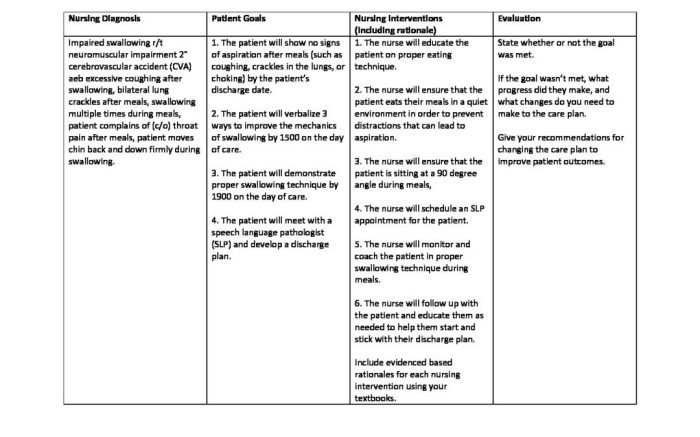
The nursing diagnosis for a patient with a hiatal hernia is impaired gastric emptying related to increased intra-abdominal pressure.
Defining characteristics of impaired gastric emptying include nausea, vomiting, abdominal distension, and constipation.
Related factors to impaired gastric emptying include increased intra-abdominal pressure, decreased gastric motility, and pyloric stenosis.
Risk factors for developing a hiatal hernia include obesity, smoking, pregnancy, and certain medical conditions, such as chronic obstructive pulmonary disease (COPD) and ascites.
The differential diagnosis for a hiatal hernia includes gastroesophageal reflux disease (GERD), peptic ulcer disease, and esophageal cancer.
Nursing Interventions: Nursing Diagnosis For Hiatal Hernia
The goal of nursing interventions for a patient with a hiatal hernia is to reduce intra-abdominal pressure and improve gastric emptying.
Nursing interventions include:
- Elevating the head of the bed
- Avoiding tight clothing
- Losing weight
- Quitting smoking
- Taking medications to reduce stomach acid
- Performing abdominal exercises to strengthen the abdominal muscles
The expected outcomes of nursing interventions include:
- Reduced intra-abdominal pressure
- Improved gastric emptying
- Relief of symptoms
Patient Education

Patient education is an important part of managing a hiatal hernia. The nurse should educate patients about the causes, symptoms, and treatment options for a hiatal hernia.
The nurse should also provide patients with instructions on how to make lifestyle changes to reduce their risk of developing a hiatal hernia, such as losing weight, quitting smoking, and avoiding tight clothing.
Patient education materials can be found on the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) website.
General Inquiries
What is the most common symptom of a hiatal hernia?
Heartburn is the most prevalent symptom associated with hiatal hernia.
Can a hiatal hernia be cured?
While lifestyle modifications and medications can alleviate symptoms, surgical intervention may be necessary in severe cases to correct the hernia.
What are the risk factors for developing a hiatal hernia?
Obesity, chronic coughing, and increased abdominal pressure are significant risk factors for hiatal hernia formation.